Sentia Health’s Electronic Medical Record Demonstration
You’ve heard the talk, let’s see the walk
Introduction
Normally we talk about healthcare and health insurance in the United States but today is a little different. We are going to take a look at exactly how we have solved the healthcare crisis. That will involve a bit of background information including the idea, the risks and benefits and the execution. We will demonstrate how this Electronic Medical Record (EMR) will shave about half the cost from health insurance with streamlining and automating the insurance process, and how to eliminate about half of the remaining cost by providing a health and wellness program that offers the patient health insurance discounts for scientifically demonstrated healthy living, giving it “teeth.” That means we are expecting a 50% savings for the patient immediately and 75% off for all of us eventually as the population gets healthier and adopts our system. This plan won’t work, however, if the EMR is unusable by practitioners. You are finally going to get to see it in action.
Background
In 2005 we at Sentia were engaged with a little company called LivingWell Health Solutions that provided patient education to employees of self-insured companies in an effort to lower their total health insurance bill. The supposition is that healthier employees will use less healthcare. Since 84% of healthcare spending in the US funds chronic, behavior-based, avoidable disease, this seems at least plausible. One idea they had was to put a nurse practitioner on-site to take care of bumps, bruises, general questions and check ups, Avoiding the expensive round trip to the doctor, insurance company, claims/coding, and all the moving parts of the US healthcare system. It was an early attempt at Direct Primary Care (DPC), for the self insured company.
What we needed, then, was a viable way for the nurse practitioner to document the care she was providing. The company was leaning toward the old standby, paper. Remember this is before HIPAA and HITECH, so paper was an option, but as a technologist, I put the kibosh on that. We needed an EMR.
One of the Nurse Practitioners had suggested that I take a look at SNOMED_CT, so I did. It seemed tailor made for what we were trying to accomplish with several million concepts and adequate to document the entire patient encounter without ICD or CPT codes that had been suborned and bent to a use that they were inadequate for. SNOMED does have crosswalks to both ICD and CPT for near automatic interoperability with legacy insurance companies.
Today, SNOMED_CT is provided by the NIH as a part of the Unified Medical Language System (UMLS). The UMLS has been translated into UMLS Metathesaurus Browser It also includes the VSAC, the Value Set Authority Center and RxNorm, the national drug database. This is literally a one stop shop for everything you need to discuss medicine and care.
A few years later, I realized that it wouldn’t take much, just a couple of tables in the database, to fully integrate health insurance into the application. It had always bothered me that some business guy was sitting in a office somewhere hundreds of miles away dictating that his company would only pay your claim if it was “coded" to his dumb specifications. This invented an entire manual infrastructure of taking the doctor’s notes and translating them in the CPT and supporting ICD codes. Who did these people think they were? So I decided to implement policies that associate patients to procedures and automate the entire process. That took less than a weekend.
We detail all that so we can say this: This is a well considered, well designed, well executed application that is quite literally better than anything on the market today for the reasons of standardization, streamlining and automation. There are several ‘enterprise’ pieces that are beyond the scope of this discussion, but rest assured that the logging and redundancies are there to make this application robust and extensible. Nobody else is using the UMLS. Everyone else uses some proprietary code set (you don’t need or want codes) that generally look like Epic or Cerner. We even have the crosswalks to translate down to those legacy EMR applications. Also, since we have this universal code set, we have a universal EMR. That actually makes the EMR problem solvable.
Epic, Cerner and Athena solved it, you say. Well, yes and no. The other EMR vendors can’t exchange information with their proprietary code sets. The other vendors charge hundreds of millions of dollars for a hospital installation. Epic made $4.6 billion last year, and they only have 7300 clients worldwide, so you divide one by the other and figure out what a hospital is paying per year. One of the reasons for the expense is that they are simply doing it wrong. They have a separate module with separate training for each specialty. That means they have 135 different separate modules with different, separate code and different, separate installations. This is why it is wrong. This is why they are so expensive. This is why they need tens of thousands of employees to maintain their applications.
We, at Sentia have one universal standardized code set, one page that represents the patient encounter, and requires no training to use.
The Demonstration
Here is what you tuned in to see. We are only going to give you an overview in the interest of time. You will see all the modules and we can give you access to our test practice to stomp around in there yourselves. You won’t get the deep dive, this time. If that is required, we can do that in person.
Login and Search
Here we see the login and search process. The returned patients are particular to your practice or hospital, but you can also search worldwide and across business and political lines.
Demographics and Insurance
We aren’t going to make you watch me type in a new patient, particularly since this is our demonstration patient. Things to note here are the Address Entry Helper that reaches out to the Texas A&M Geosciences department and validates and corrects addresses so they are 100% accurate. One little architectural note here: Addresses are kept in a CONTAINS format. Earth contains countries, countries contain states and provinces, states and provinces contain cities and towns. Cities contain streets and streets contain numbers, etc. This gives us the flexibility to capture any address, even unincorporated ones, instead of having a hardcoded Address1, Address2 Address3, which doesn’t accurately represent the data we are trying to capture. For a deeper discussion my contact information is at the end of this article.
Health Risk Assessments
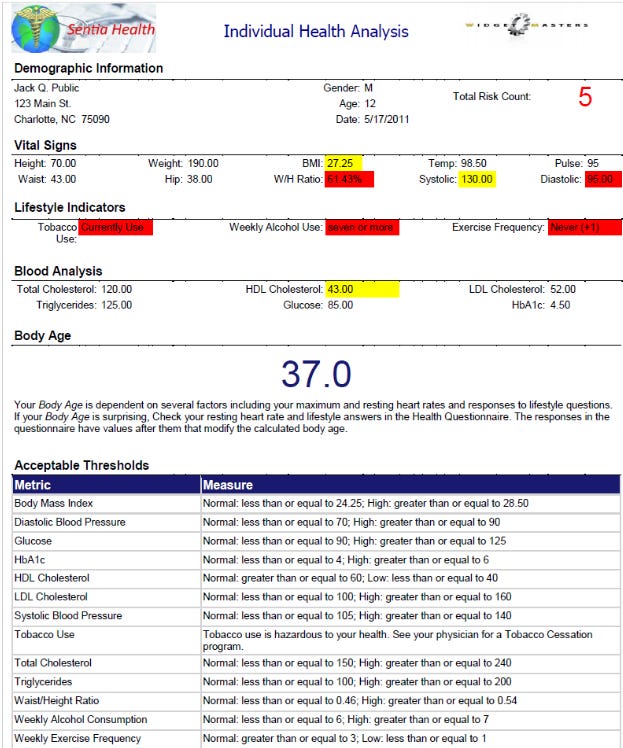
This contains all the normal blood work and clinical measurements that you would expect along with a short family and personal history section. Future plans may include adding the family history in UMLS format instead of hardcoded checkboxes for more and more flexible information. We will dive deeper into the UMLS style documentation in the Patient Encounter section later. Again, we won’t subject you to watching us fill out forms unless there is something truly different. At the end of this section, we will show the printable Health Risk Assessment Document detailing for the patient exactly what measurements are out of normal range.
Of note here is the Body Age. This is calculated based on resting heart rate and assumed maximum heart rate allowing us to calculate an oxygen uptake, and modified with behavioral considerations as shown in red. It is based on the Uth, Sørenson, Overgaard, and Pedersen equation. Patient education is automatically prescribed based on anything that is highlighted in the Individual Health Analysis.
There is also a Population Health Analysis that will detail the concerns your particular practice or hospital has, like higher than average hypertension or higher than average cholesterol and allows the practice to focus the entire population on correcting those problems. A sample of that report is available but beyond the scope of this article.
Patient Encounter (The SOAP Note)
This is where the meat of the application lives and where we will demonstrate the power of the UMLS and the structured data approach without codes and coding, while being easily human readable. We will start with the clinical measurements and lab values filled in, as above, you don’t want to watch us type into a form. Notice as we go that the notes are very lean, and “just the facts.” there is no History of Present Illness as they would be in a classical SOAP Note, because that would have been captured in a previous encounter. There is no discussion of allergies as those would have been captured in another section of the application. Contrary to your training, these things, while germane, only serve to muddy the notes and ensure that the downstream practitioner will NOT read them.
Subjective
Here we see the user entering basically what the patient tells us. Notice how we can modify any concept, usually a finding, by clicking the ellipsis to the left of the modifier value. In this case we even denote that the pain seemingly moved from the hypogastric region to the lower right abdominal quadrant. Then we will add loss of appetite due to abdominal pain and nausea.
Objective
Here we will see what the clinician actually finds and can measure. Notice the extensive use of the modifier section.
Assessment
There isn’t much here, just the conclusion of the practitioner's findings, in this case the patient has appendicitis.
Plan
While this looks simple, there is a lot to unpack here. First, notice that the covered procedure is in green and has a number attached to it. This is the payment from us (or your self-insured employer) with no adjudication, no delays, no denials and no negotiation. This is a take it or leave it number. If you as a practitioner don’t want to take our payment, we will remove you as a recommendation. There are no networks, but we do recommend practitioners with whom we have done business before. Of note, this plan has one policy that belongs to this patient. The plan also only covers this one procedure. While this application has been in production and used at a regional hospital in North Carolina, this part is a prototype, so don’t put too much stock in the dollar value for the procedure performed. We will flesh out the plans as we get more information and as necessary. The lesson here is that this is all data driven and all configurable.
SOAP Note Conclusions
While this may seem a little bit cumbersome for documentation, This becomes the template for future diagnoses of appendicitis. It is quite literally one click documentation. If you don’t like this one, you can mark another instance of this same diagnosis as a template. I didn’t like the fact that the patient said the pain moved. So I probably wouldn’t use this one.
That said, we gain a number of things by doing documentation this way.
First, this is just as fast or faster than writing or typing.
Second, there isn’t all the fluff as in a traditional soap note, only structured data. In looking for a suitable note to duplicate, I ran across a template that was taught in nursing school that started “Patient presents with screaming and crying in pain.” Sure, and sad, but irrelevant in scientific documentation.
Third, because this is structured data, and it is standardized, we can begin to associate things like symptoms with diagnoses. There won’t be any more Dr. House beating his head with his cane trying to come up with a diagnosis. He will just ask the EMR to show him diagnoses for people with these symptoms and then be able to go look at anyone’s chart that presented with those symptoms worldwide.
Fourth, we only get the facts. I believe that this has been taught wrong for years. I believe it was taught that way to give a mini history with every patient encounter because, paper. Nobody was going to go down to the archives to look at previous cases, because they just didn’t have time. So, you get “screaming in pain” and “lives with mother” and “denies fever/chills, etc.”
One Click Documentation
As discussed above, this will serve as a template for all appendicitis diagnoses going forward unless another case of appendicitis is marked as a template. These templates are refreshed on a rolling six weeks average. Yes, this caters to the general practitioner so that influenza will rise to the top during the flu season and can be documented with one click. Here is a screenshot of the dropped down top diagnoses list box ready to do all your documentation with a single click:
Here is an example showing that exact thing:
Automatically Prescribed Patient Education
As the Health Risk Assessment is documented, the system will automatically prescribe patient education based on clinical measurements and lab results. Clearly the practitioner does not need this education so this is a good time to mention that everything we have seen, and will see, is available to the patient on a read only basis. This gives the patient the ability to actually read his or her medical records for veracity and to correct any errors. All of the prescription of patient education is done in the background by the system, but let’s take a look at what the patient sees when they log in to see it.
Things to notice here, though you can’t see it, the education opens in a new tab. Some of the education is just that, like excessive drinking. The other two examples both have one or more ‘temperature gauges’ that show the comparison between your measurement and the standard range, and the graphic of the normal range on the right. Below that we will generally have a problem statement and a solution statement, or what the patient can do to rectify the situation s/he finds himself or herself in. There are also links to further definition documentation to explain some of the more esoteric points of medicine, like cholesterol.
The system detects and logs when the patient opened the education and how long s/he spent reading it. This means we, as the insurance company, have the opportunity to offer a tiny discount simply for reading the education. Remember that 84% of health expenditures in the US are spent on chronic, behavior based, avoidable disease. If the patient actually follows the directions in the documentation and gets better, or at least not worse, then they earn large, double-digit discounts. This shifts the burden of behavior based, avoidable, chronic disease to those who don’t do the things necessary to stay healthy and makes them pay for consuming more than their fair share of healthcare.
DICOM, Imaging and Documents
Built right into the system is the ability to upload and view saved images and documents including DICOMs. We at Sentia believe DICOMs are an abomination as the only difference is that they have a header with the patient’s information that is a holdover from the paper days when a film might fall out of a folder and get lost. This is no longer the case, but I digress. The next video will show how easy it is to upload and view documents and images.
There is also the ability to automatically generate growth charts but showing those is beyond the scope of this document and our test patient has aged out of needing those in any case. We can send examples of these on request.
There is a second DICOM viewer built into the telemedicine portion of the EMR but that is currently under re-development as the technology selected has been deprecated. We are working diligently to get this back up and running. The big claim to fame of this secondary viewer is that the participants can not only see each other and the image, but are both able to draw on it to highlight structures worthy of closer inspection and show a reticle to highlight things worth noting. This will be rebuilt shortly, and we will be able to show it off.
Secure Email
Many of you may have wondered why you can’t just send email to your patients. That is because email is sent in clear text across the internet. That makes it amazingly insecure and not HIPAA compliant. We have built in a secure ‘email’ system into our application so you can collaborate with your colleagues and patients securely.
Self Scheduling
The patient can log in and schedule themselves for any available slot with their practitioner at any time. The next vignette shows a patient doing exactly that.
This operation results in an email to the patient and the practitioner’s time being blocked off. Our scheduling program does NOT block out room time so the front office staff will actually have to do the room assignments. We automate the things that are automatable, no more, and no less.
Patient Lists
Finally, the main reason we built the documentation system the way we did was to be able to generate patient lists. Here we will demonstrate looking up people (from our practice) that have had an appendectomy. We know of at least one.
Next, we are going to combine several things, in this case hypertension as it pertains to diastolic blood pressure and pregnancy to filter out our patients who show symptoms of Gestational Hypertension. Any of these few dozen boxes can be combined and the UMLS data can be stacked up as we did in documenting our test subject’s appendicitis.
Conclusions
While there are a few other administrative details we could show off, we have hit the high spots that practitioners will care about. Here are some general conclusions
We have proven that a universal EMR is not only viable, but necessary to more forward
We have proven that the UMLS is the only viable source of data for that EMR and that nobody else uses it.
We have proven that by integrating health insurance with the EMR we can save about half from the cost of health insurance and eliminate everything the insurance company currently requires the practice and patient to do and eliminate the associated costs.
We have shown a way to automate all the patient documentation by using the first instance of a diagnosis as a template or marking a subsequent instance as a template.
We have shown a way to put ‘teeth’ into patient education that will cause our population to reduce the instance of chronic, avoidable, behavior based disease to the OECD average for mortality for saving another 25% of the total cost of health insurance.
We have shown a way to research all things medicine by associating symptoms, diagnoses, measurements and lab results into real information.
We have shown a way to share DICOMs and imaging across the internet.
We have shown a secure ‘email’ system allowing real communication with colleagues and patients.
We have shown a way to engage the patient and to have them come to this application as their default for all things medicine, including scheduling.
We have shown a way to use one-click reporting to automate things that need reports like the individual Health Analysis, the Population Health Analysis, and the Population Current v. Prior Analysis. These are simply the beginning of the reporting.
The only other thing we really need to address to completely save the US healthcare system is to identify waste and fraud at the hospital level. We are working on this currently with a completely new design for an Enterprise Resource Planning (ERP) style Practice Management System (PM) that includes every piece that affects the finances of the practice or hospital. You can see the details of that here.
We have built a comprehensive health information system to keep the patient healthy and on the right track with the ability to incentivize healthy living. This system includes the automation of the health insurance industry completely. We have designed and are currently building the ERP style PM system. Implementing this system should be fairly simple and will completely revolutionize the way healthcare is paid for, saving countless lives. We have shown a way to use this system to make the best healthcare system in the world also the most efficacious and the most affordable.
If you liked what you read contact us here, on our site, SentiaHealth.com, our parent company SentiaSystems.com, or send us an email to info@sentiasystems.com or info@sentiahealth.com.